Back to Atlases main
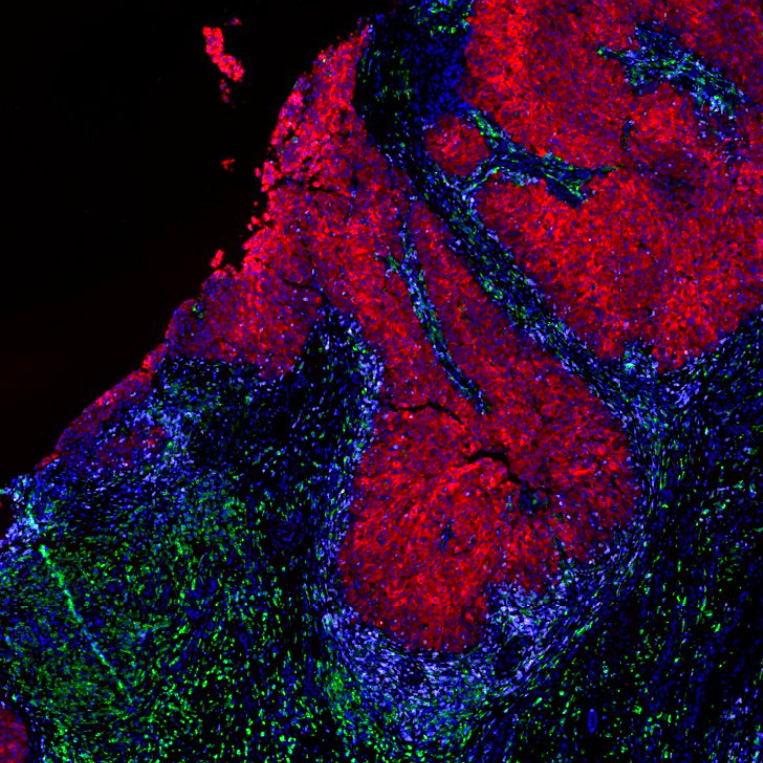
Melanoma Pre-Cancer and Progression Atlas
Melanoma is an increasingly common type of cancer that often becomes metastatic when quite small, making melanoma a dangerous disease. Routine surveillance of the skin, followed by removal of lesions suspicious for cutaneous melanoma, is common in many developed countries. However, surveillance and staging are not perfect and some dangerous lesions slip through. Moreover, individuals with less access to healthcare do not benefit from regular monitoring and some times of melanoma (e.g. acral lentiginous melanoma) are underdiagnosed and undertreated, particularly in people of color. By improving our understanding of the sequence of molecular events that drive melanoma, the Melanoma Atlas will improve diagnosis, staging, and disease management.
Melanoma is noteworthy in that it can be treated both with targeted therapy (inhibitors of the RAF and MEK kinases for the ~50% cutaneous melanomas carrying BRAF mutations) and with immunotherapy (inhibitors of the PD-1 and CTLA-4 checkpoint proteins). Understanding precisely why these therapies achieve longer and deeper remission in some patients than others is not only relevant to understanding targeted and immunotherapy in general, but also to improving patient care–choosing among treatment options at the level of individual patients is not always straightforward. The importance of understanding the high responsiveness of melanoma immunotherapy is increasing since many other types of solid cancer have proven to be much more resistant to immune therapy.
Publications
View Narrated Data
View Curated Data
View Automated Data
Key Questions
- What are the earliest events that lead to melanoma? How can we detect melanoma precursors and eradicate them?
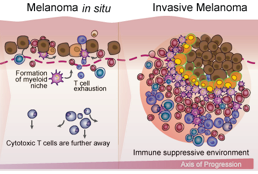
- What are the key events in melanoma progression? Why does the immune system successfully clear many pre-melanomas but fail to stop others?
- How can we use this information to recognize melanomas that are at high risk of progressing to metastatic disease?
- What molecular events allow some melanoma cells to escape therapy and survive as residual disease?
Principal Investigators
- Genevieve Boland, MD PhD, Section Head of Melanoma/Sarcoma Surgery, Massachusetts General Hospital
- Christine Lian, MD, Associate Professor of Pathology, Brigham and Women’s Hospital
- David Liu, MD, MPH, MS, Assistant Professor of Medicine, Dana-Farber Cancer Institute
- George Murphy, MD, Director of Dermatopathology, Brigham and Women’s Hospital
- Sandro Santagata, MD PhD, Associate Professor of Pathology, Brigham and Women’s Hospital and Harvard Medical School
- Dirk Schadendorf, MD, Director of the Department of Dermatology, University Hospital Essen
- Eugene Semenov, MD MA FAAD, Instructor of Dermatology, Massachusetts General Hospital
- Peter Sorger, PhD, Professor of Systems Biology, Harvard Medical School
Publications
Highly multiplexed 3D profiling of cell states and immune niches in human tumours.
Yapp C, Nirmal AJ, Zhou FY, Wong AYH, Tefft J, Lu YD, Shang Z, Maliga Z, Montero Llopis P, Murphy GF, Lian C, Danuser G, Santagata S, Sorger PK. (2025).
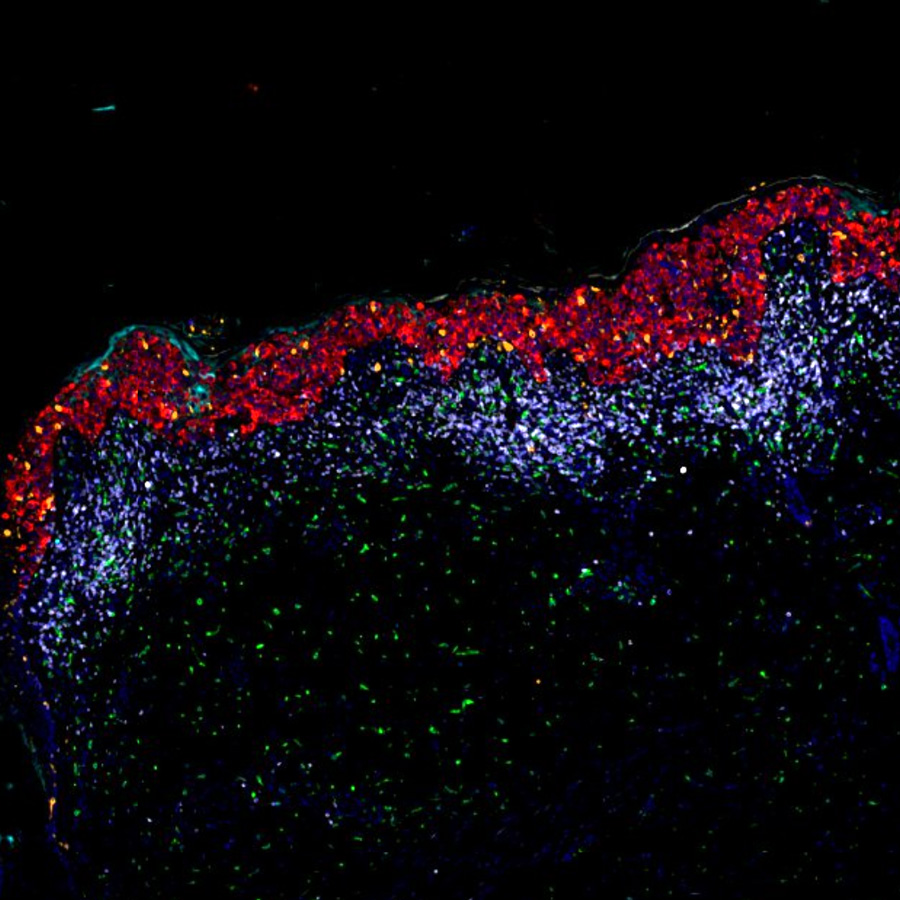
Spatial determinants of tumor cell dedifferentiation and plasticity in primary cutaneous melanoma
Vallius T, Shi Y, Novikov E, Pant SM, Pelletier R, Chen YA, Tefft JB, Johnson AN,...Sorger PK. (2025).
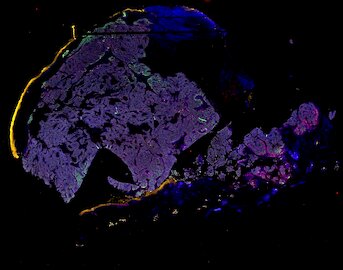
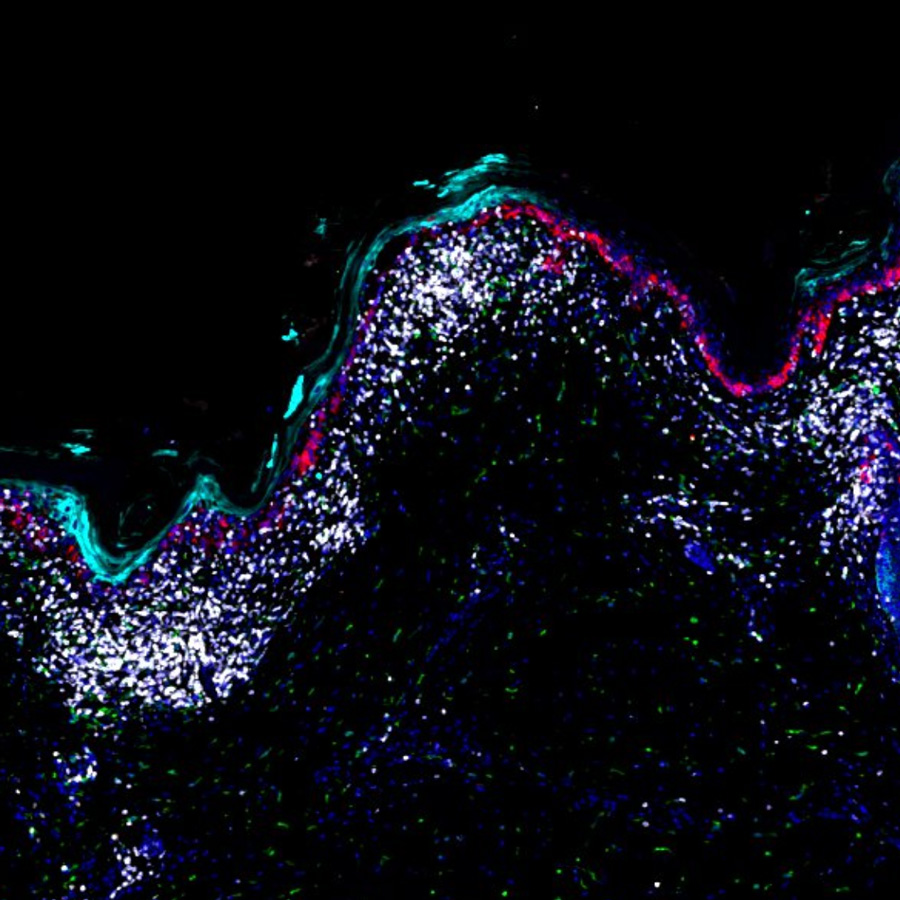
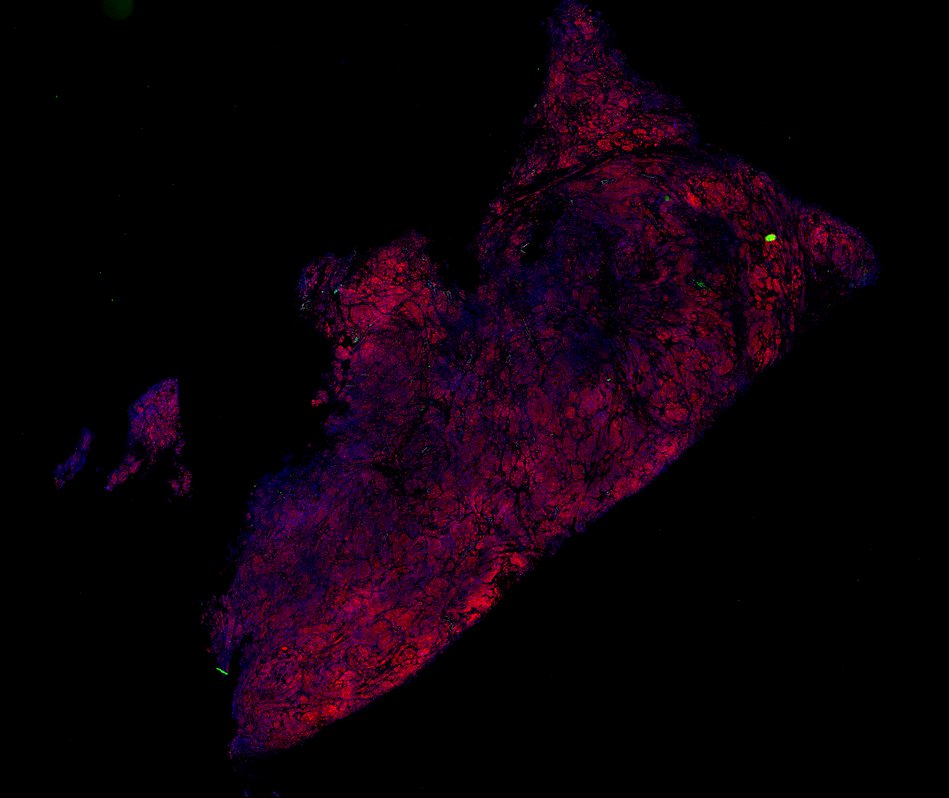
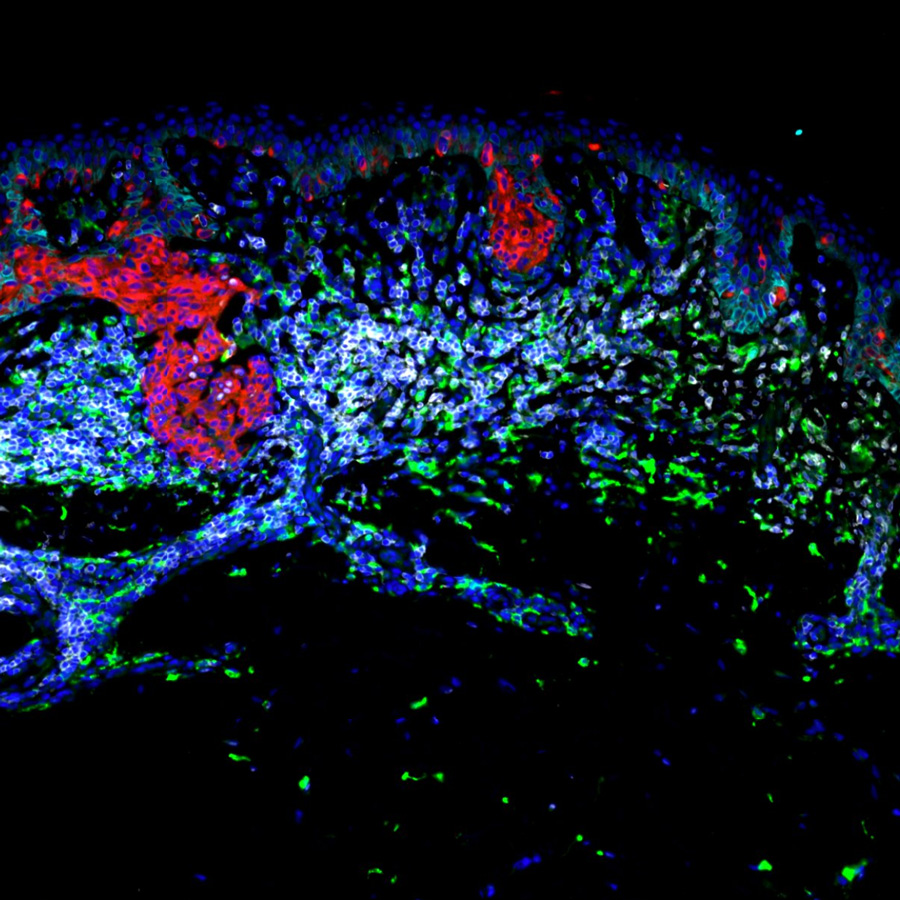
The spatial landscape of progression and immunoediting in primary melanoma at single cell resolution.
Nirmal AJ, Maliga Z, Vallius T, Quattrochi B, Chen AC, Jacobson CA, Pelletier RJ,... Lian CG, Murphy GF, Santagata S, Sorger, PK. (2022)
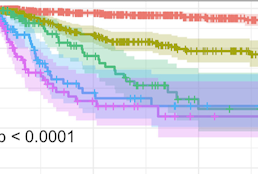
Evolution of delayed resistance to immunotherapy in a melanoma responder.
Liu D, Lin J-R, Robitschek EJ, Kasumova GG, Heyde A, Shi A, Kraya A,... Boland, GM. (2021).
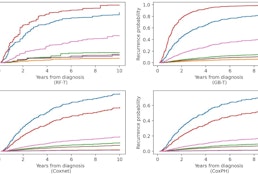
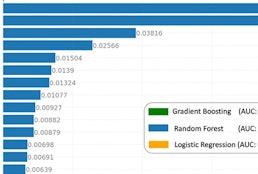
Prediction of early-stage melanoma recurrence using clinical and histopathologic features.
Wan G, Nguyen N, Liu F, DeSimone MS, Leung BW, Rajeh A, Collier MR, Choi MS,... Semenov YR. (2022).
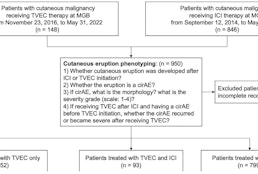
SpatialCells: automated profiling of tumor microenvironments with spatially resolved multiplexed single-cell data.
Wan G, Maliga Z, Yan B, Vallius T, Shi Y, Khattab S, Chang C, Nirmal AJ, Yu K-H, Liu D, Lian CG, DeSimone MS, Sorger PK, Semenov YR.(2024).
Narrated Minerva Stories
Narrated stories use multi-step narrations and annotations to walk a viewer through key features of the data. Narrated stories distill the multidisciplinary knowledge encompassed by each dataset into a single product that grounds the scientific analyses in the underlying data and metadata. Click the Minerva story icon for an interactive view of the full-resolution images.
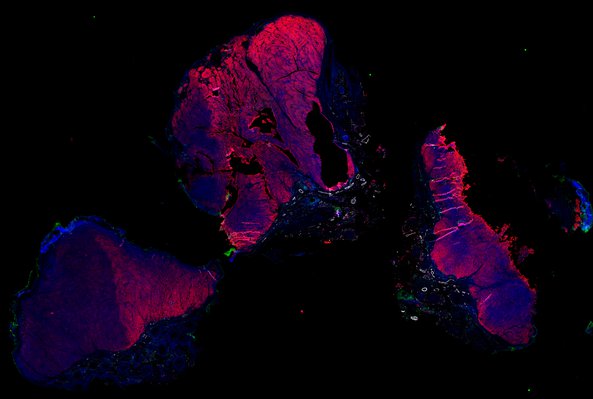
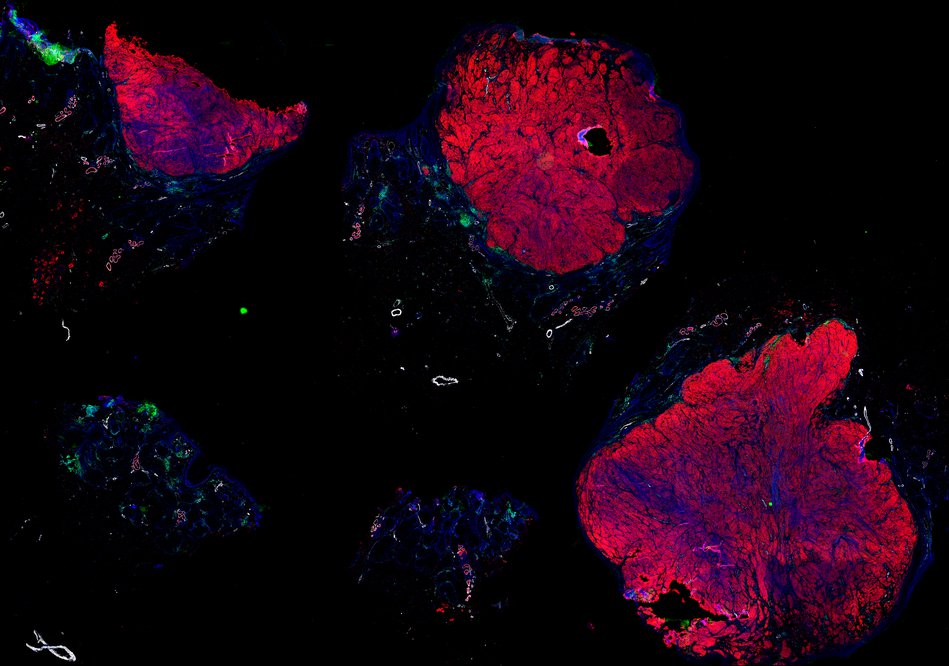
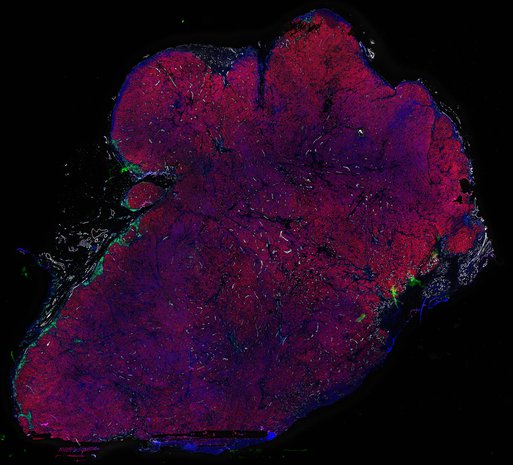
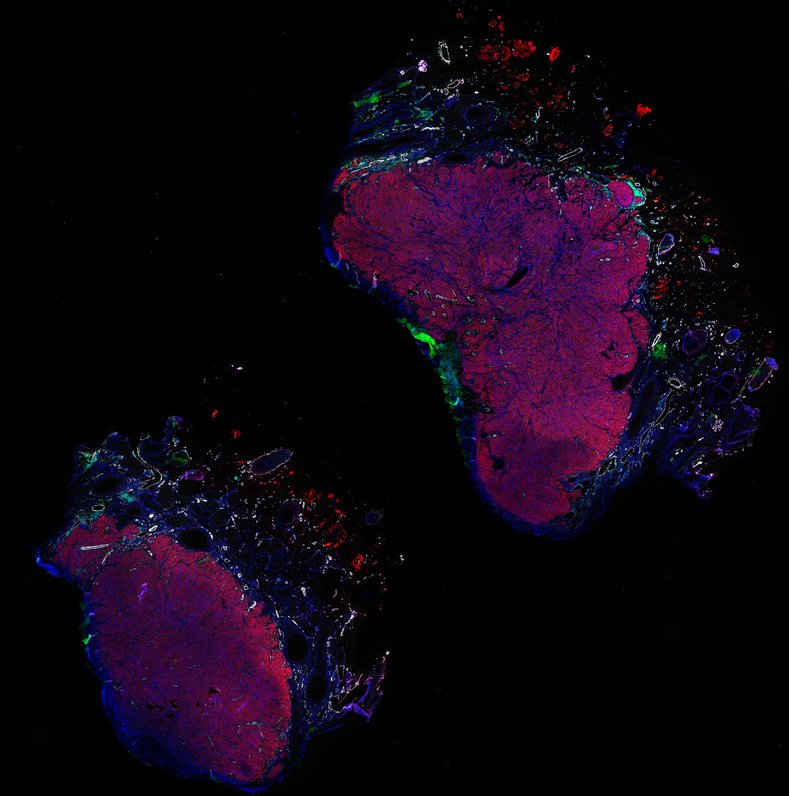
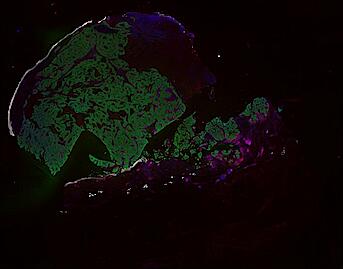
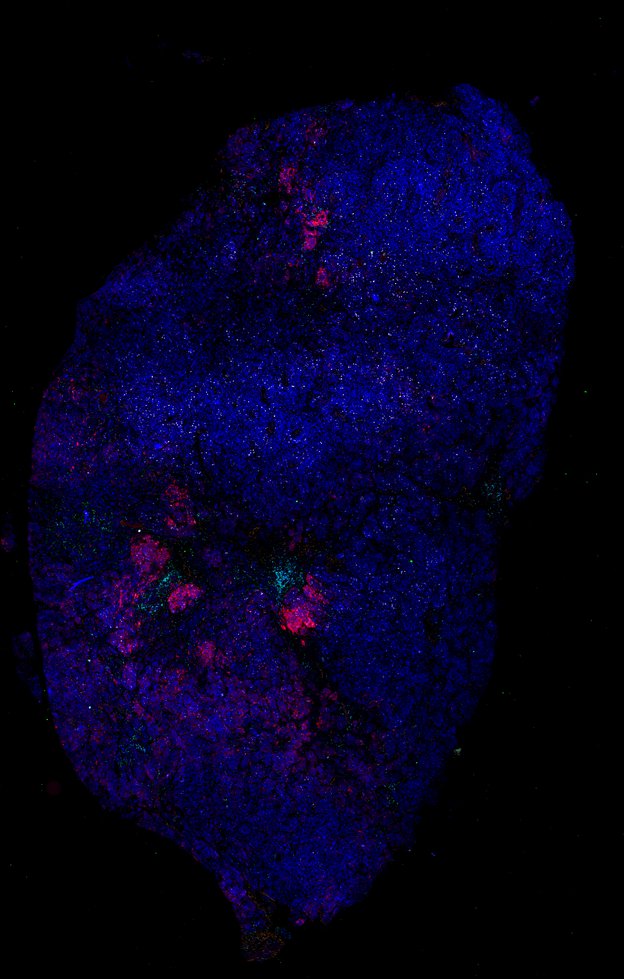
Deep Exploration of a Primary Melanoma (MEL 1 Full Story)
Introduction to the MEL Atlas (MEL 1 Abstract)
Two Ways of Immune Evasion in Early Melanoma (for non-experts)
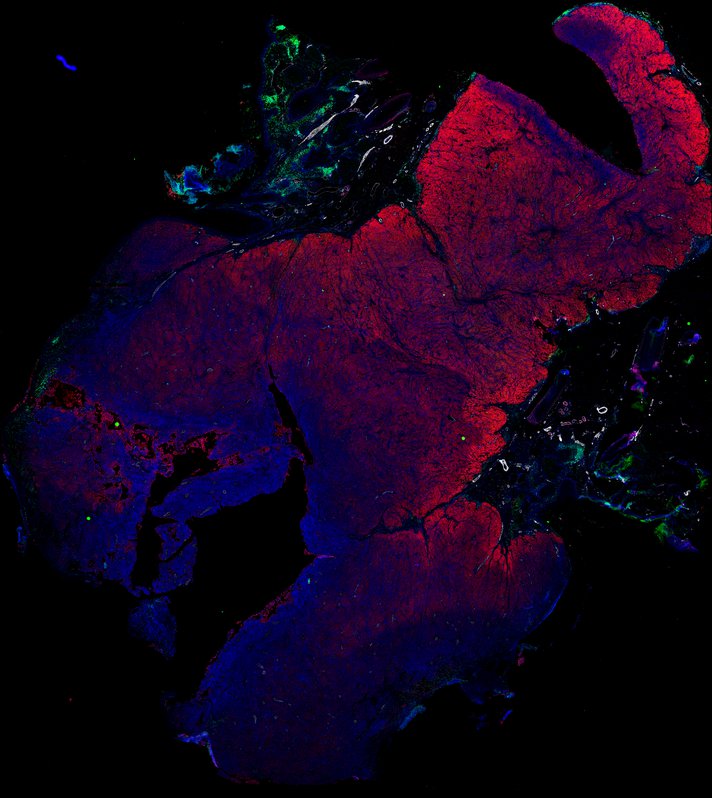
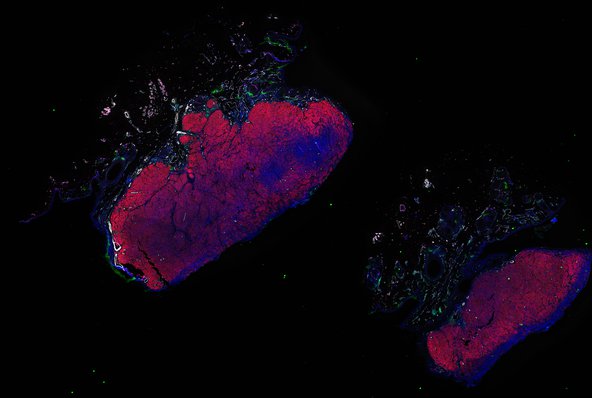
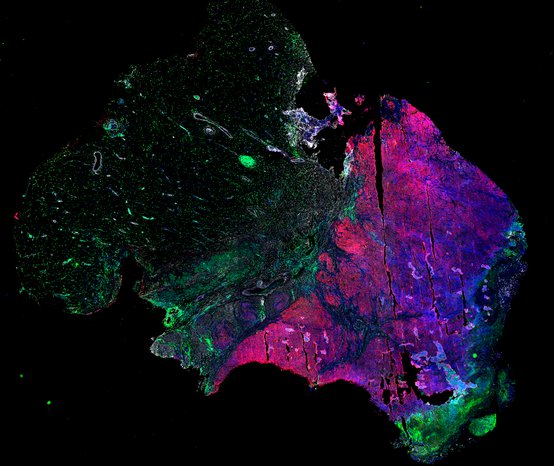
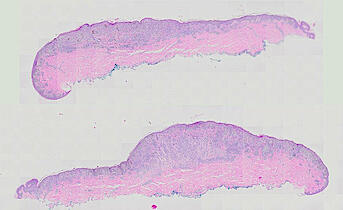
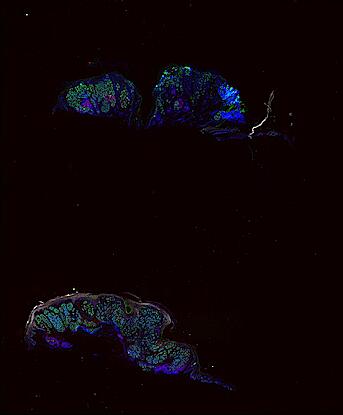
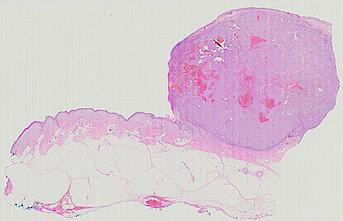
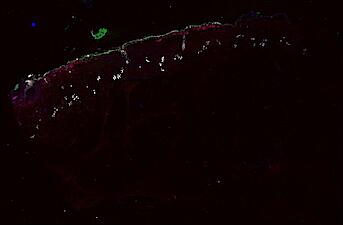
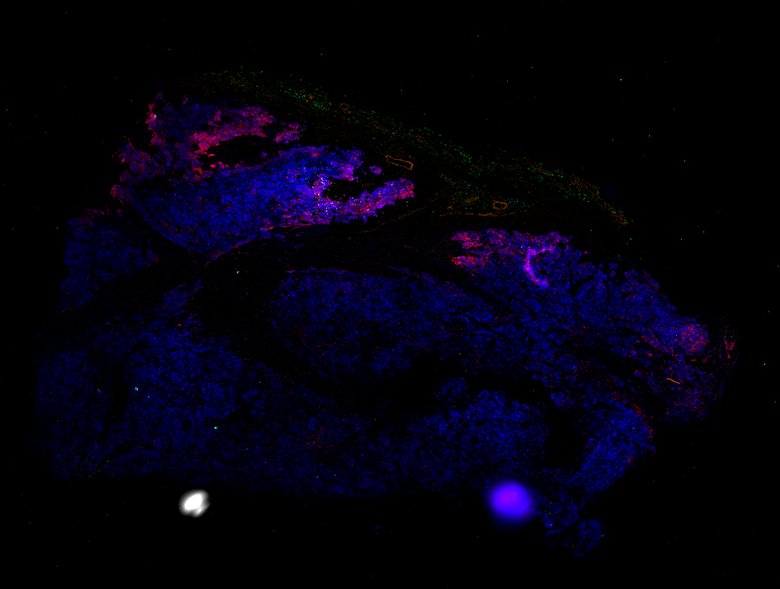
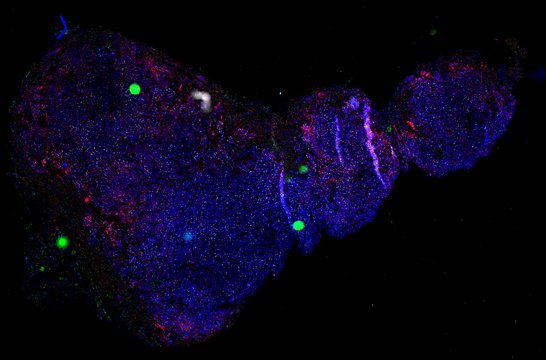
Patient 2 - Melanoma in situ, invasive melanoma, precursor field and inflammatory regression
Curated Minerva Stories
Curated stories provide access to images that have undergone a quality control step to remove failed markers, ensure appropriate channel intensity settings, and provide metadata about the underlying sample and image. Click the Minerva story icon for an interactive view of the full-resolution images.
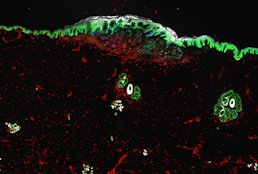
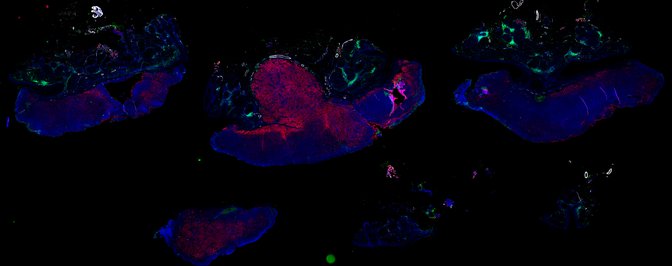
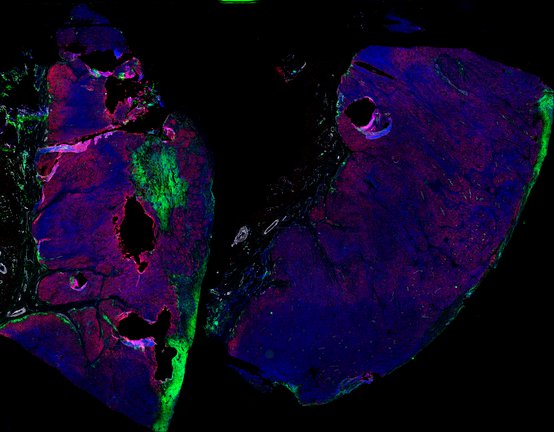
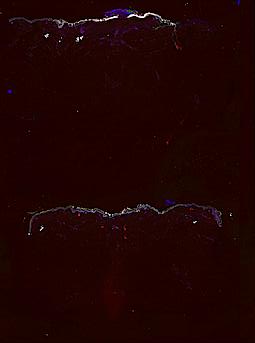
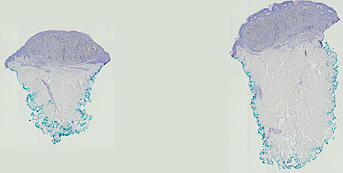
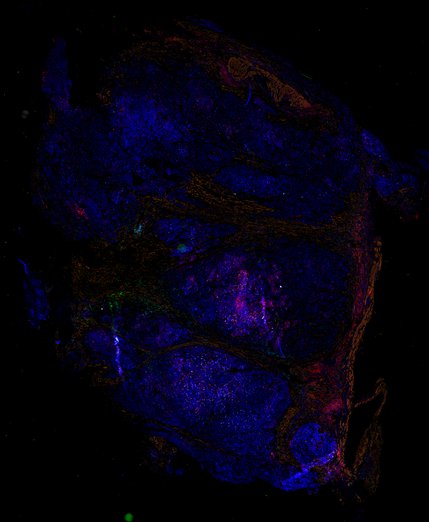
Melanoma in-situ with 3D imaging
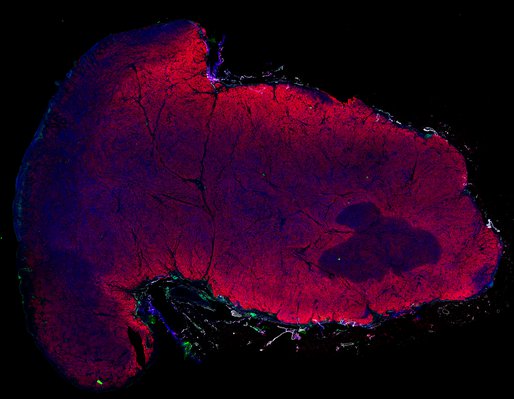
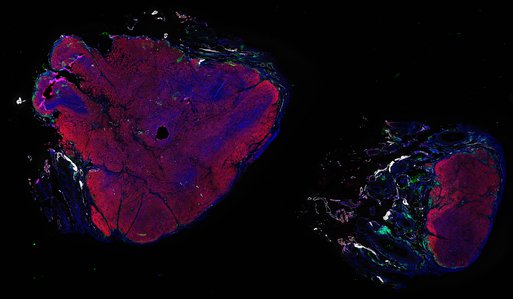
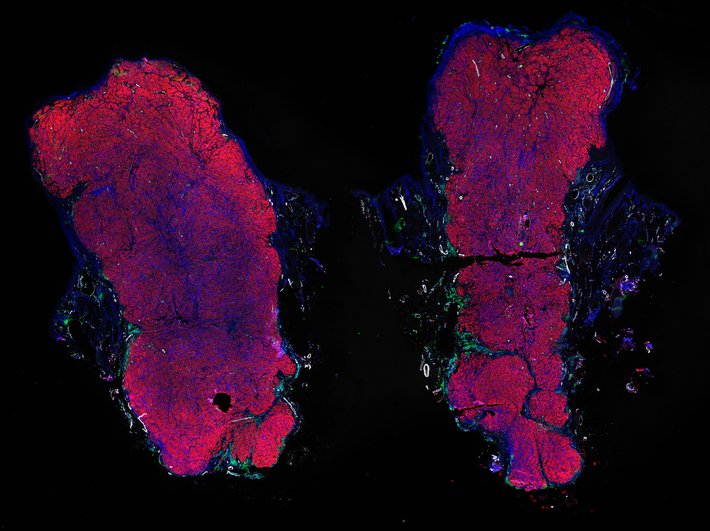
Melanoma VGP - 3D CyCIF - LSP13625
Melanoma MIS - 3D CyCIF - LSP13625
Melanoma VGP - 3D CyCIF - LSP13626
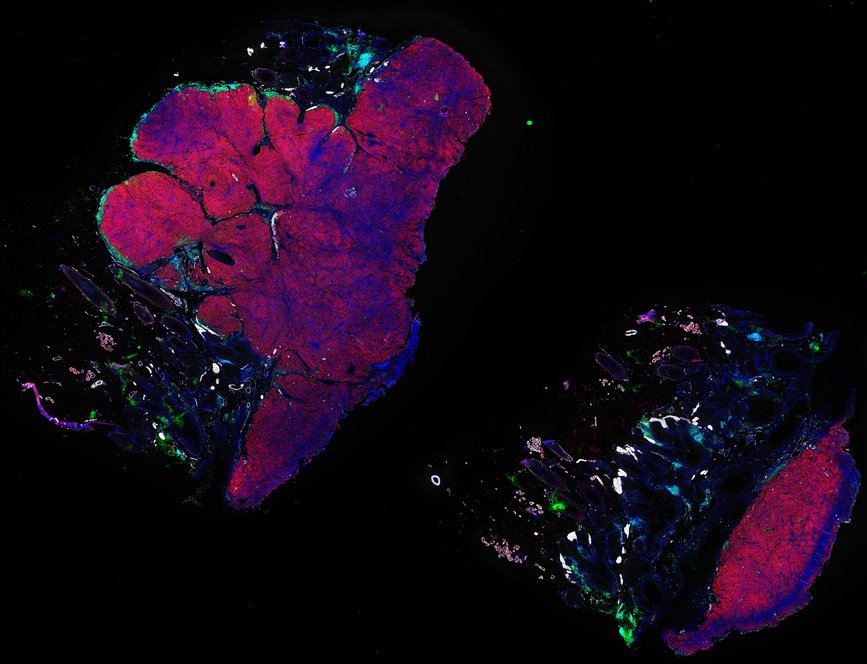
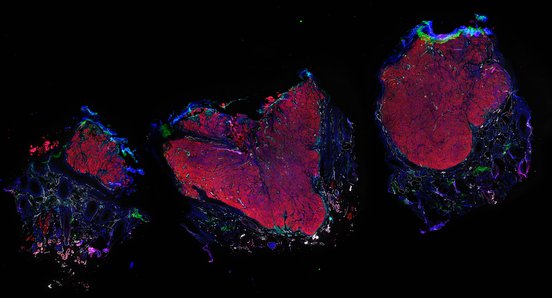
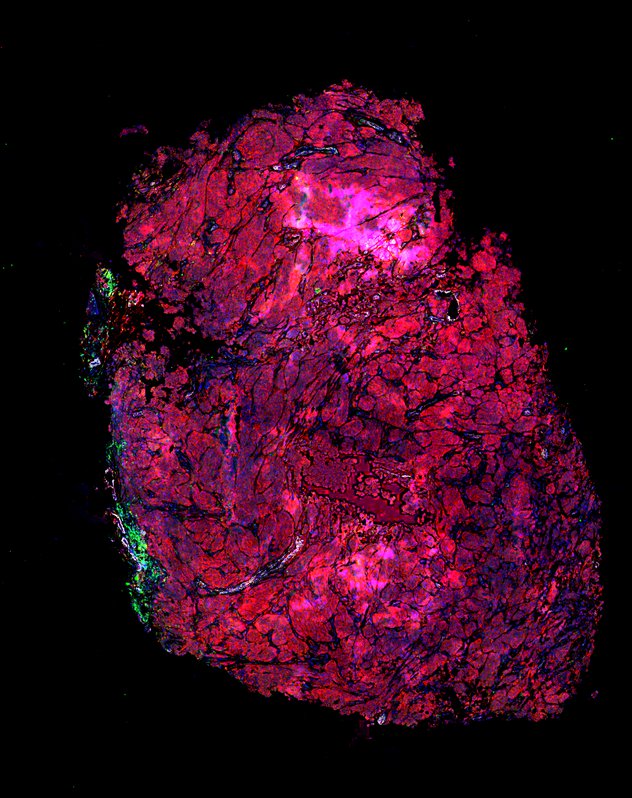
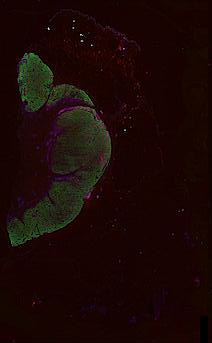
Metastatic melanoma - 3D CyCIF - LSP22409
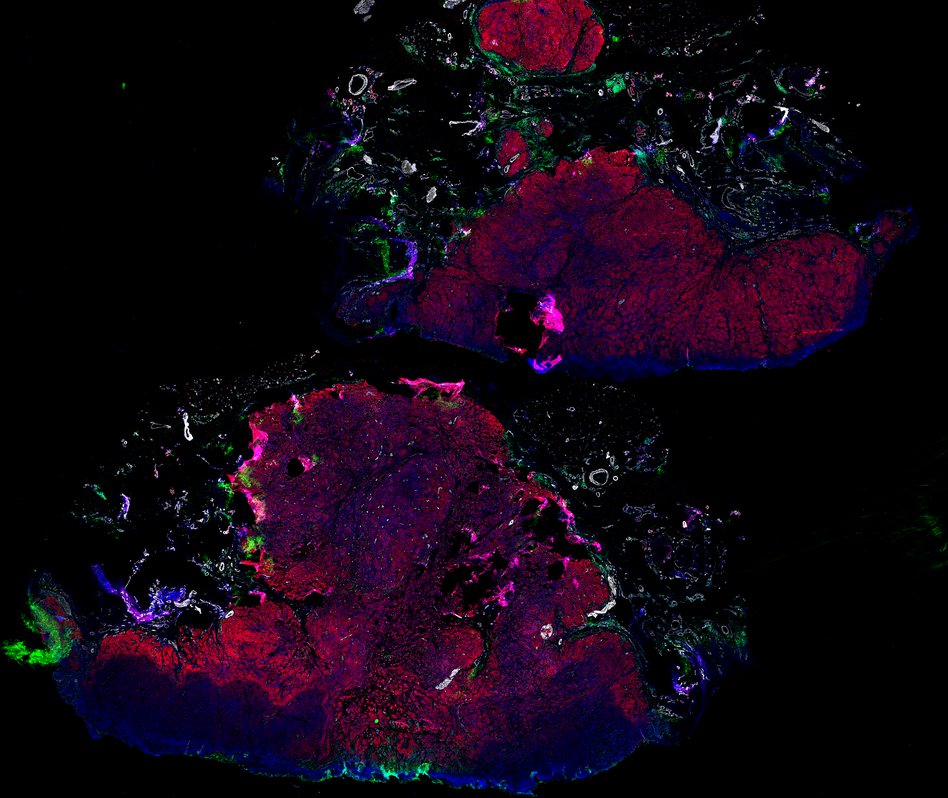
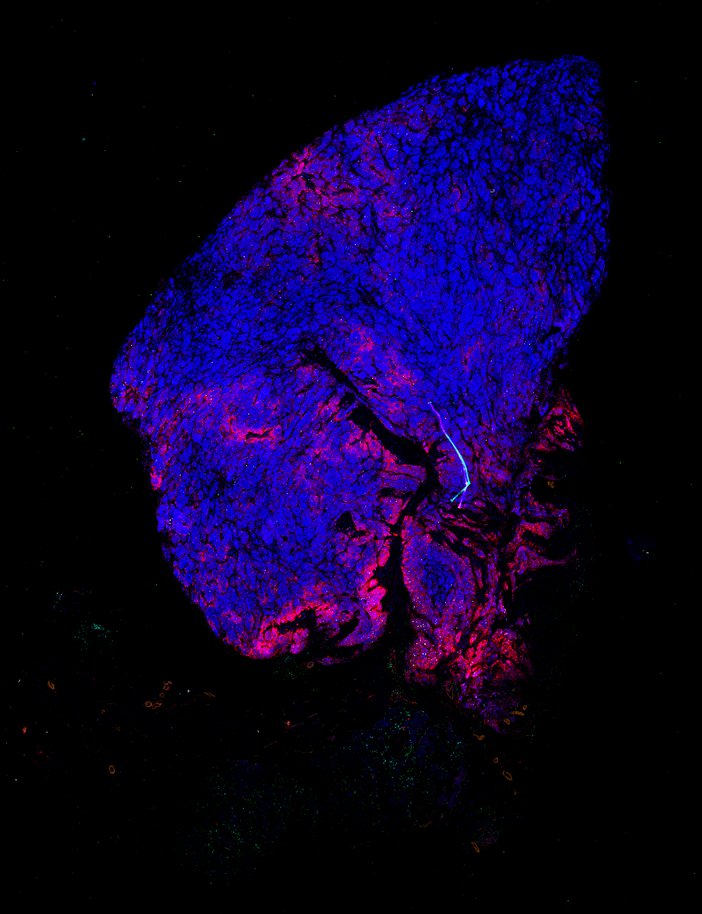
Cell State Dependent Effects of Bmal1 on Melanoma Immunity and Tumorigenicity
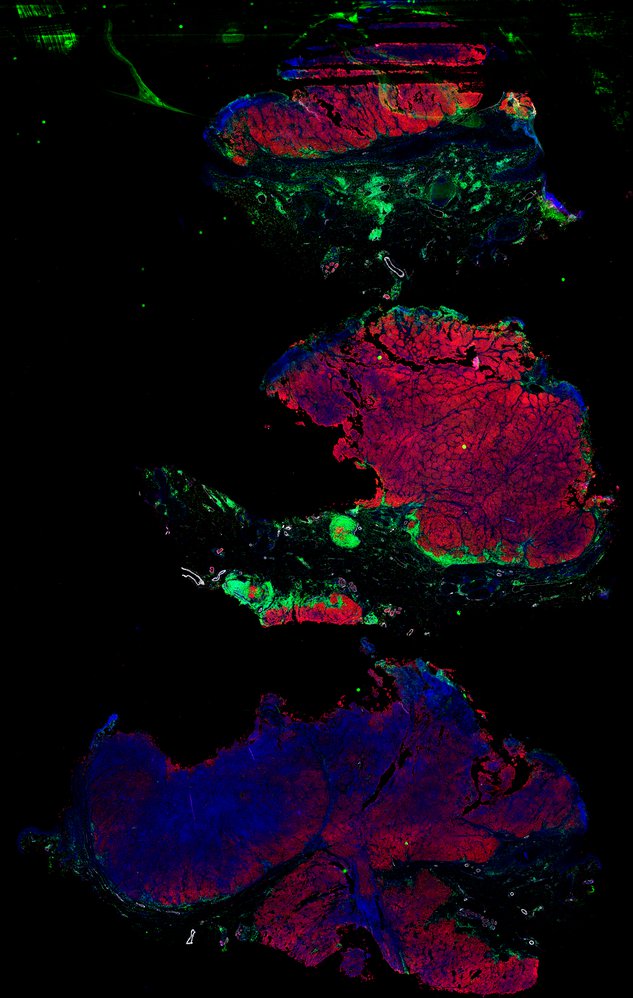
Longitudinal study of metastatic melanoma - Day 92 - Skin, right upper lip (T21)
Longitudinal study of metastatic melanoma - Day 92 - Skin, left neck (T20)
Longitudinal study of metastatic melanoma - Day 92 - Skin, left groin (T19)
Longitudinal study of metastatic melanoma - Day 76 - Skin, left leg (T15)
Longitudinal study of metastatic melanoma - Day 76 - Skin, right nasal labial fold (T17)
Longitudinal study of metastatic melanoma - Day 76 - Skin, right neck (T16)
Longitudinal study of metastatic melanoma - Day 62 - Skin, left wrist (T14)
Longitudinal study of metastatic melanoma - Day 62 - Skin, right neck (T13)
Longitudinal study of metastatic melanoma - Day 39 - Skin, left arm (T12)
Longitudinal study of metastatic melanoma - Day 39 - Skin, posterior neck (T10)
Longitudinal study of metastatic melanoma - Day 39 - Skin, left scalp (T11)
Longitudinal study of metastatic melanoma - Day 39 - Skin, right scalp (T9)
Longitudinal study of metastatic melanoma - Day 27 - Skin, right ear (T8)
Longitudinal study of metastatic melanoma - Day 27 - Skin, left brow (T7)
Longitudinal study of metastatic melanoma - Day 27 - Skin, chin (T5)
Longitudinal study of metastatic melanoma - Day 27 - Skin, upper lip (T6)
Longitudinal study of metastatic melanoma - Day -22 - Skin, nasal labial fold (T4)
Longitudinal study of metastatic melanoma - Day 1028 - Jejunal resection (R1)
Longitudinal study of metastatic melanoma - Day 109 - skin, left ring finger (T22)
Longitudinal study of metastatic melanoma - Day 83 - skin left shoulder (T18)
Longitudinal study of metastatic melanoma - Day 1862 - skin left neck (R3.2)
Longitudinal study of metastatic melanoma - Day 1849 - skin left neck (R3.1)
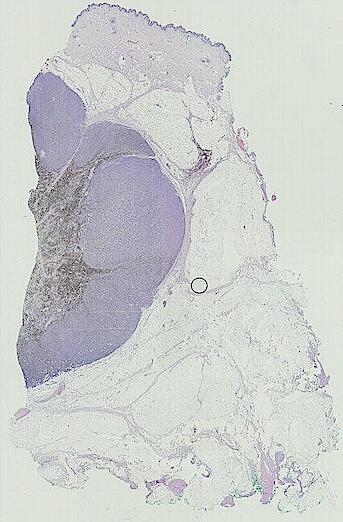
Metastatic melanoma lesion and adjacent benign tissue (Figure 2)
Automated Minerva Stories
Automated stories provide basic image viewing with automatic rendering settings, enabling rapid, lightweight sharing of highly multiplexed images, without download. Click the Minerva story icon for an interactive view of the full-resolution images.
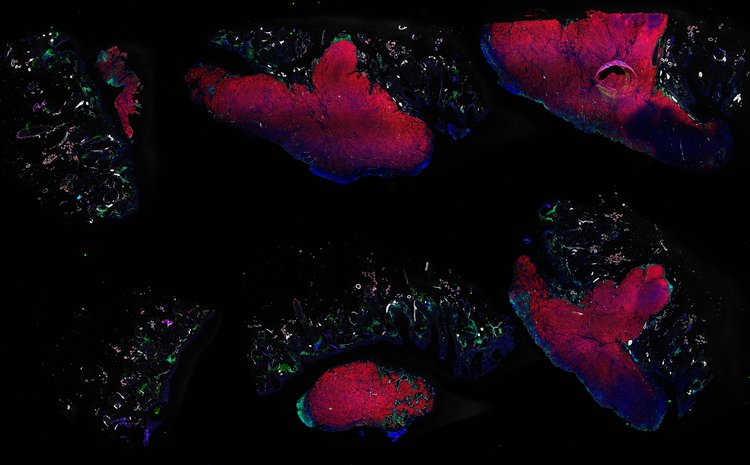
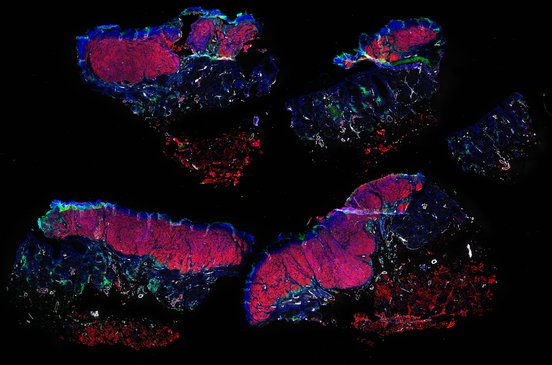
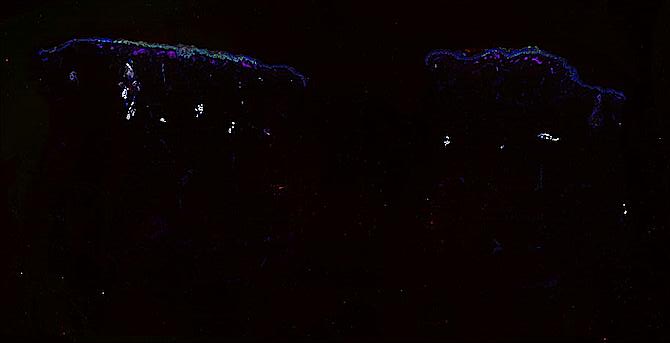
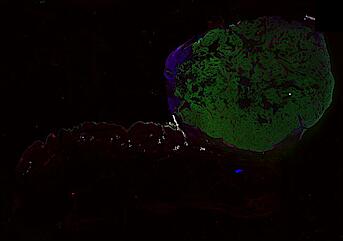
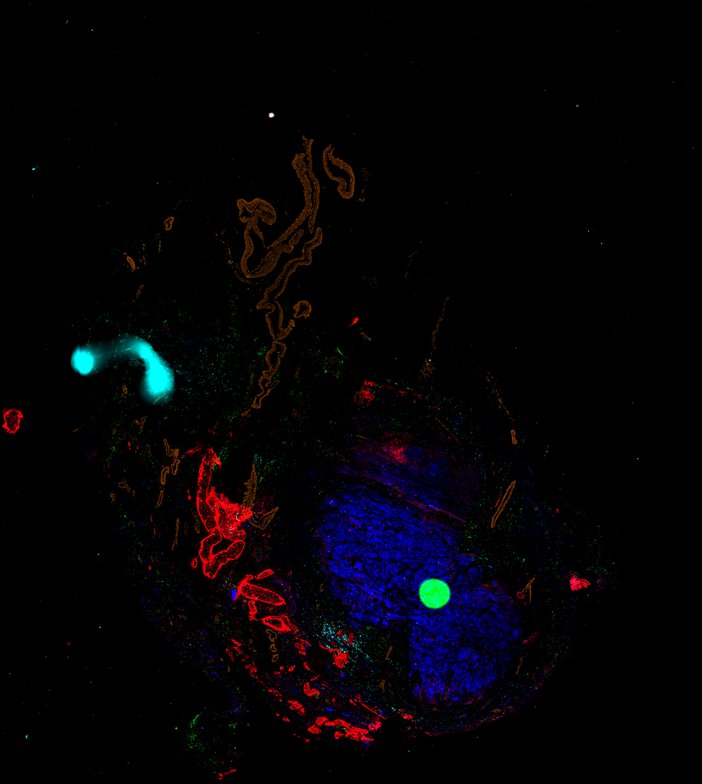
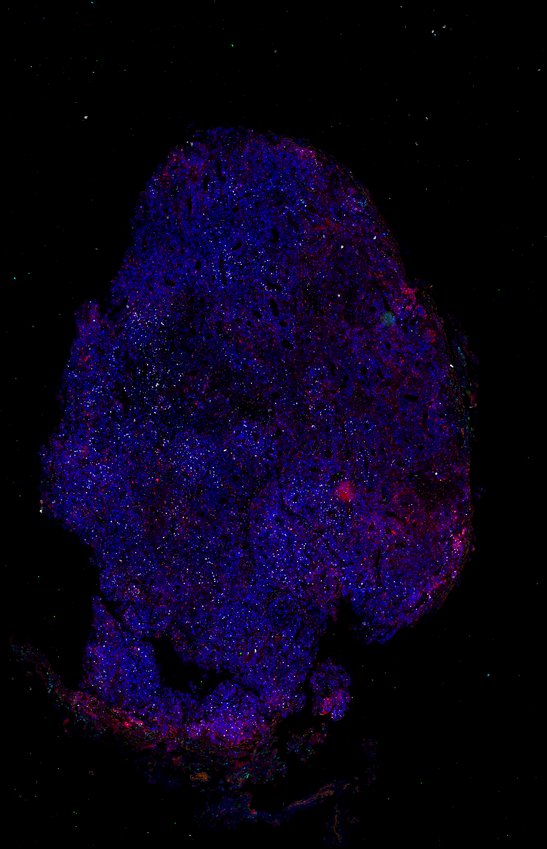
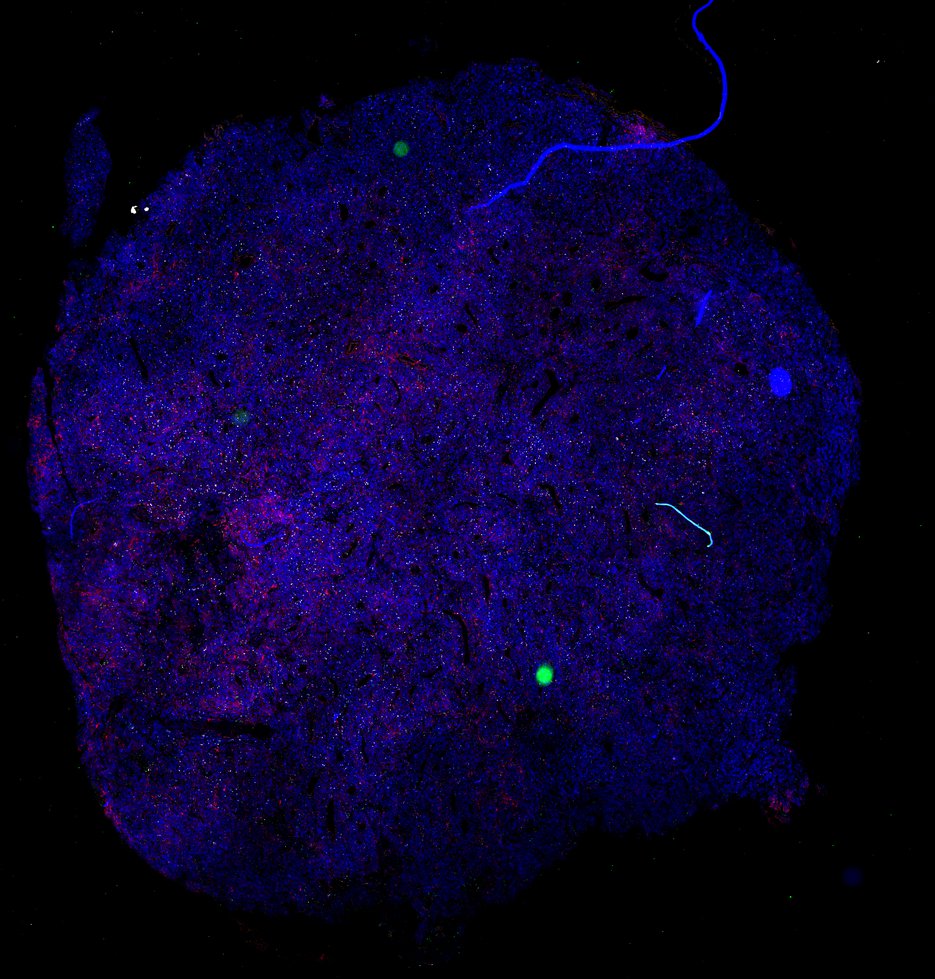
MEL13-2-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
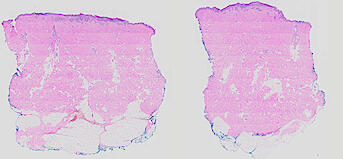
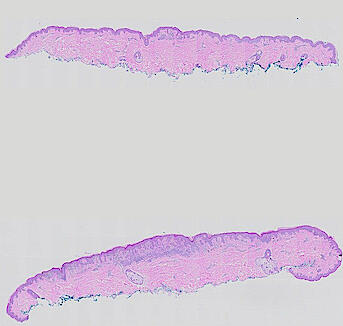
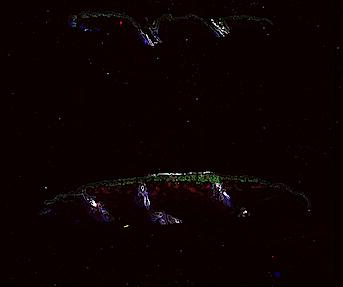
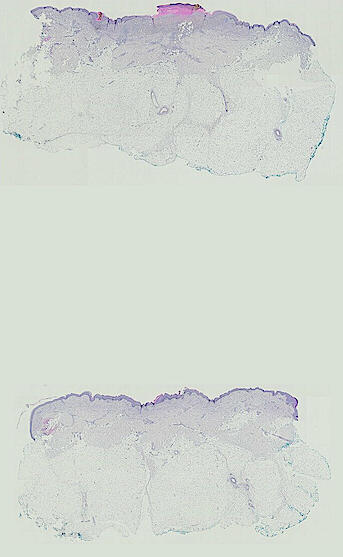
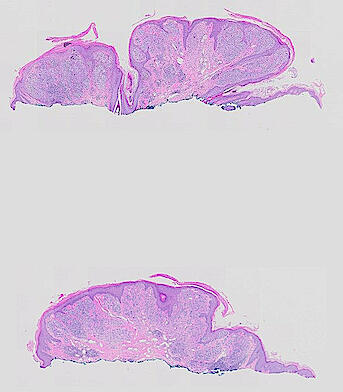
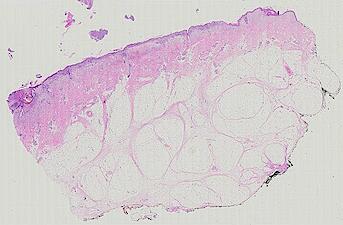
MEL13-2-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL13-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL13-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL12-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL12-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL11-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL11-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL10-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL10-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL09-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL09-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL08-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL08-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL07-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL07-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL06-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL06-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL05-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL05-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL04-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL04-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL03-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL03-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL02-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL02-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
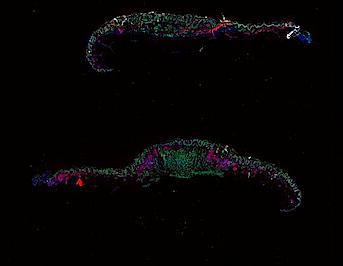
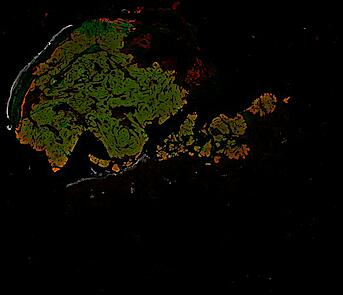
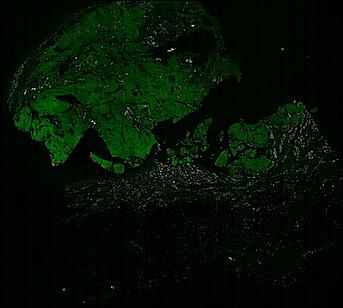
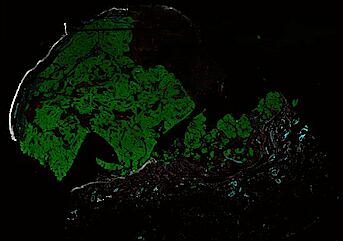
MEL01-3-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
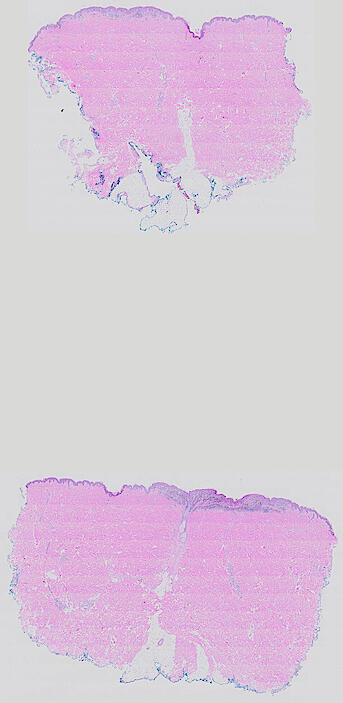
MEL01-3-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-2-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-2-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-6 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-5 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-4 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-3 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-1 - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
MEL01-1-0 - H&E - overview - Nirmal, Maliga, Vallius, Sorger et al., 2021
Longitudinal study of metastatic melanoma - Autopsy - Right adrenal (AV1)
Longitudinal study of metastatic melanoma - Autopsy - Subcutaneous lesion, left temporal bone (AS4)
Longitudinal study of metastatic melanoma - Autopsy - Subcutaneous lesion, left scalp (AS3)
Longitudinal study of metastatic melanoma - Autopsy - Subcutaneous lesion, left inguinal region (AS2)
Longitudinal study of metastatic melanoma - Autopsy - Subcutaneous lesion, left mastoid (AS1)
Longitudinal study of metastatic melanoma - Autopsy - Lung, left lower lobe (AL4)
Longitudinal study of metastatic melanoma - Autopsy - Lung, left upper lobe (AL3)
Longitudinal study of metastatic melanoma - Autopsy - Lung, right upper lobe (AL2)
Longitudinal study of metastatic melanoma - Autopsy - Lung, right lower lobe (AL1)
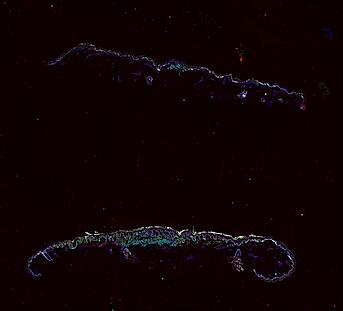
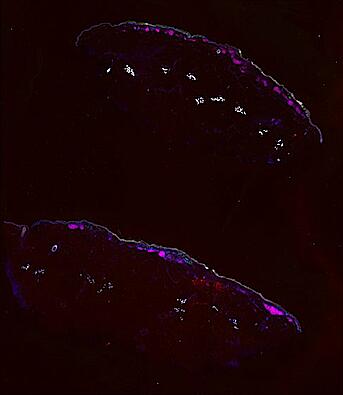
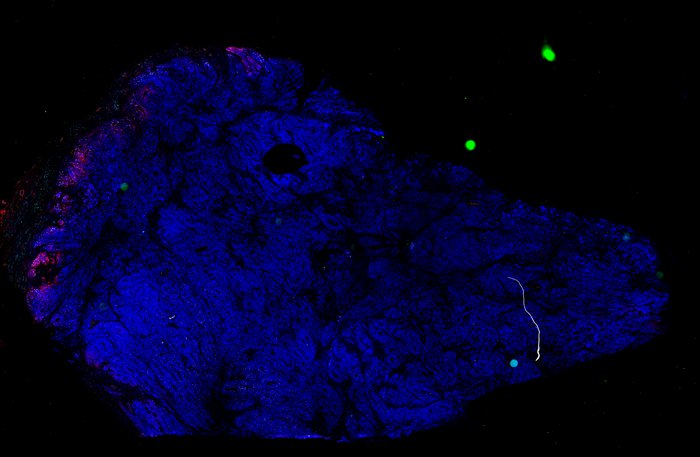
Patient 1 - Melanoma with precursor fields
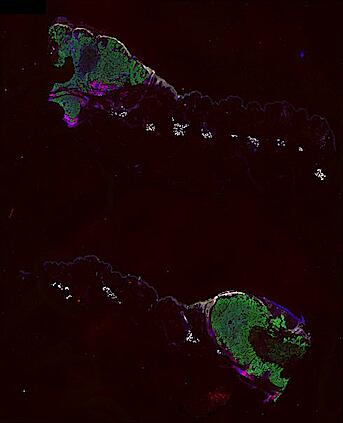
Patient 2 - Inflammatory regression and brisk TILs
Patient 2 - Melanoma in situ, invasive and polypoid melanoma
Funding
Research on precancers and primary melanoma is supported by the NCI Human Tumor Atlas Network as part of the Pre-cancer Atlases of Cutaneous & Hematologic Origin (PATCH) Center (Grant U2C-CA233262). HTAN aims to generate, publicly-accessible data on the spatial, genetic and epigenetic features of common human cancers and precancers. Research on advanced and metastatic melanomas are supported by the NCI Cancer Systems Biology Program (Grant U54-CA225088). Additional support is provided by the Ludwig Center at Harvard Medical School and the Ludwig Institute for Cancer Research.